Senior doctors claim that it is difficult for the NHS to provide all cancer patients with safe and effective care.
In all four UK countries, there is a "chronic staff shortage," according to the Royal College of Radiologists, which is causing patients to wait too long for necessary examinations and treatments.
Radiotherapy and chemotherapy treatment delays are now occurring frequently, according to half of all cancer units.
A workforce strategy for the NHS in England, according to ministers, will be released soon.
Several delays have been made to the plan, which is intended to outline how the government will fill staffing gaps over the next 15 years. This has angered some in the health service.
Ministers in other parts of the UK claim that reducing cancer waiting lists is a top priority and that additional funds are being invested in personnel and diagnostic tools. .

Carol Fletcher, a South Wales resident, finally attended her routine breast cancer screening appointment in June 2022, which was long overdue.
She recalled that it took another eight weeks after her mammogram before she was informed that there might be a problem.
Since she was diagnosed with cancer, there have been additional waits for scans, tests, surgery, and chemo.
She explained that there was an additional eight-week delay in chemotherapy because she had been warned that she might not receive the results of her mastectomy immediately because there weren't enough pathologists available.
"I can't plan for the future, and my family is really suffering because of it. ".
Long before Covid, the NHS services in the entire United Kingdom struggled to meet cancer targets.
Lockdowns caused by the pandemic caused scans and treatment to be delayed, which increased the backlog.
One important goal is for treatment to begin in England, Scotland, and Northern Ireland within two months of an urgent GP referral.
Wales has a slightly different measurement because it takes both urgent and non-urgent referrals into account. .
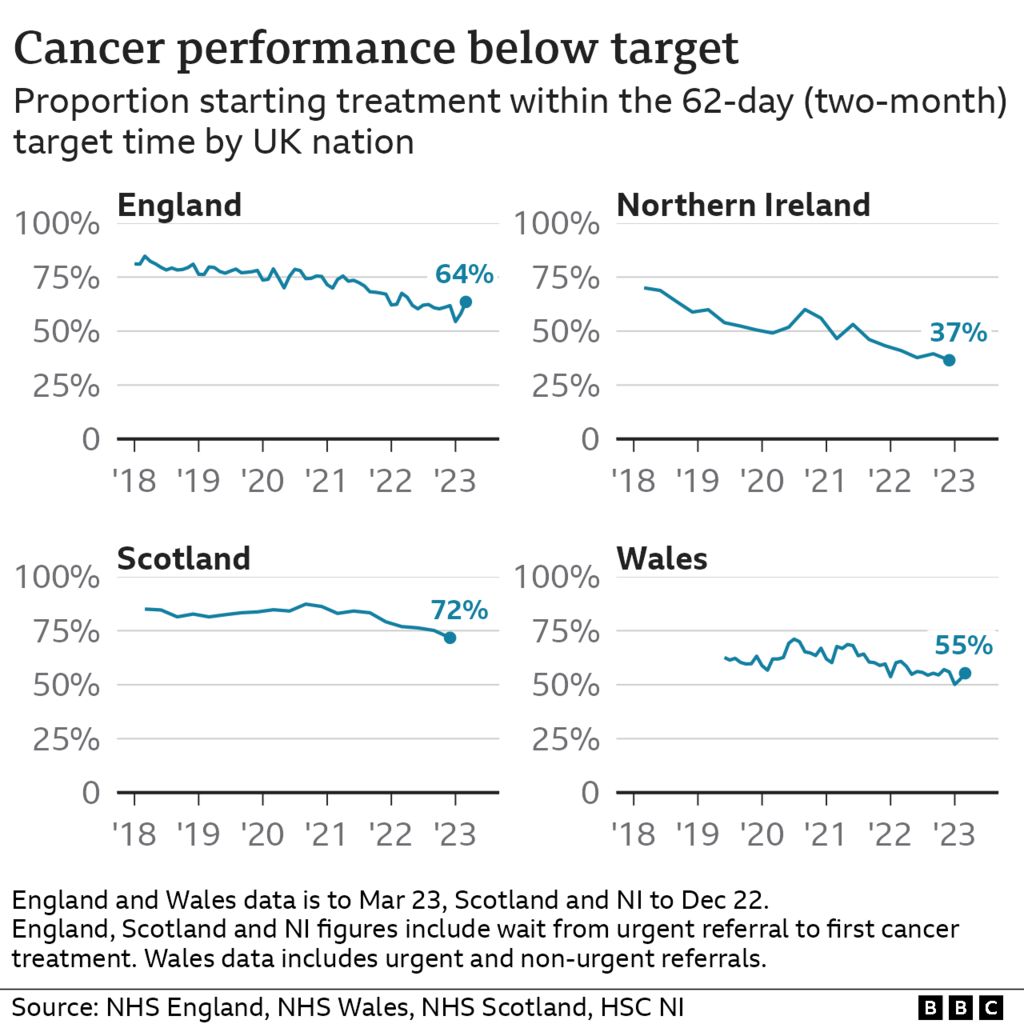
Operating at far below those levels are all four countries. Against a goal of 85%, only 64% of patients in England begin treatment in that time.
Growing delays are, in part, the opposite of a success story in medicine.
Astonishing scientific advancements in cancer treatment have given patients hope where there previously had been little hope.
Although new techniques are more complex for doctors to use, they are also more effective.
The UK population is aging at the same time, and since cancer risk is strongly correlated with age, there is a growing need for expensive scanners, as well as more staff to analyze those scans and more specialized doctors and nurses.
According to the Royal College of Radiologists (RCR), the situation is a "perfect storm," and the workforce is finding it difficult to keep up. .
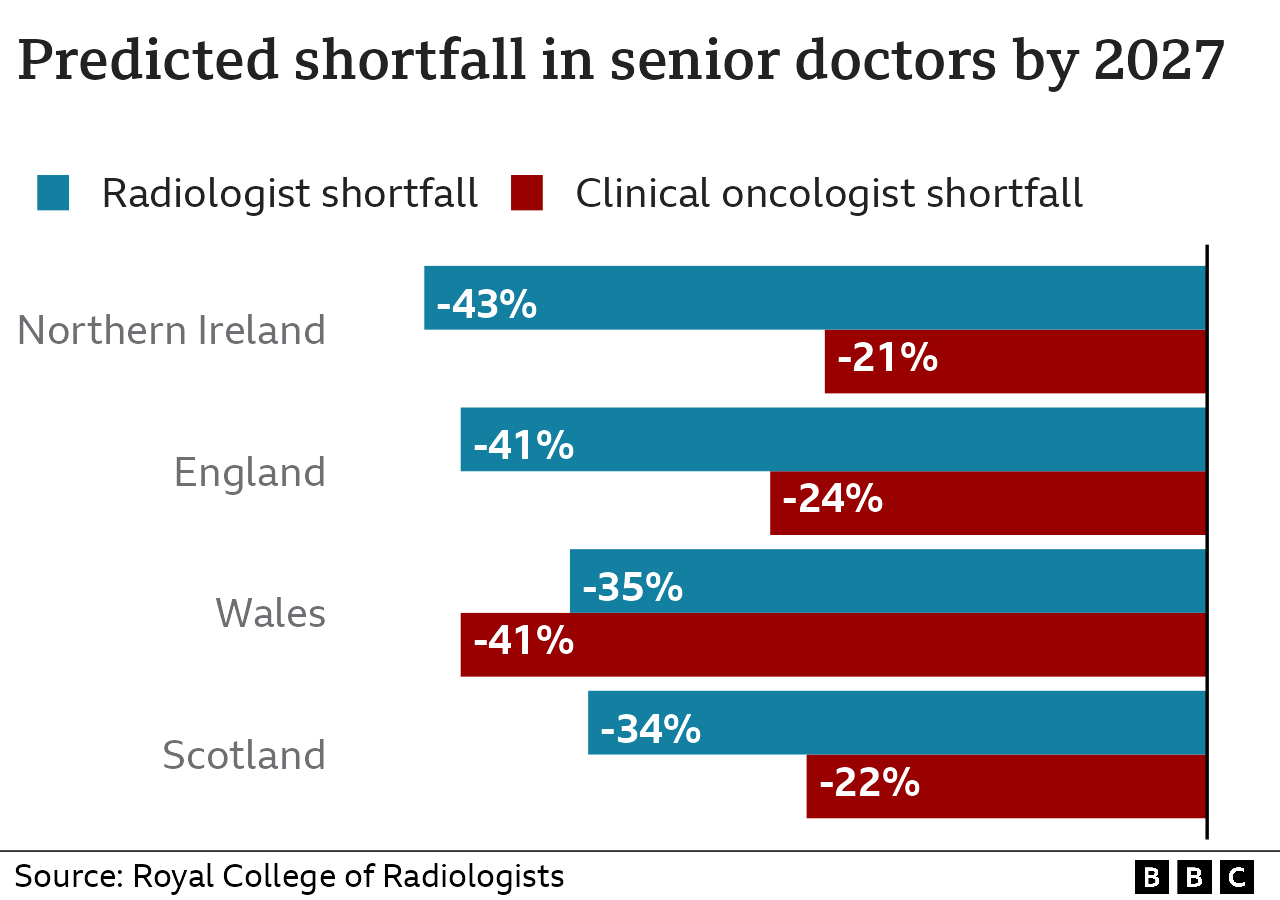
It estimates that there is currently a 15% shortage of clinical oncologists—specialist doctors who administer chemotherapy and radiotherapy—across the four UK nations.
By 2027, it predicts that this gap will increase to 25%, or a shortage of 368 full-time consultants, if nothing is done.
The scarcity of consultant radiologists—highly qualified medical professionals who analyze scans to determine the presence of cancer or track its development—is also alarming.
According to the RCR, the risk of death rises by about 10% for every month a patient delays beginning cancer treatment.
As of this year, 44 percent of cancer service managers—up from 29 percent last year—say they are "highly concerned" about patient delays, according to the organization's annual survey.
According to Dr. Tom Roques, a consultant oncologist and vice-president of the RCR, "there are examples in almost every cancer center where parts of the service just aren't running as well as we would like.".
"We frequently have to inform patients that we can't treat them as quickly or effectively as we'd like, and this is a stressful task to undertake. ".

In a motorcycle accident in November of last year, County Durham resident Kevin O'Hara, 60, broke five ribs.
A shadow near one of his kidneys was discovered during a scan of his upper body and was later determined to be cancer.
He was given the option of taking drugs to slow the tumor's growth, and in early February, he was informed that there would be a three to four-month wait before surgery could be performed.
He is still waiting for a date for his surgery even though that time period is now over.
He said, "You are waiting every day, and nothing changes.
"I get so depressed when I don't see an envelope with NHS written on the top when I get home from work and knock on the door. " .
Often ignored, there is another development in the field of cancer treatment.
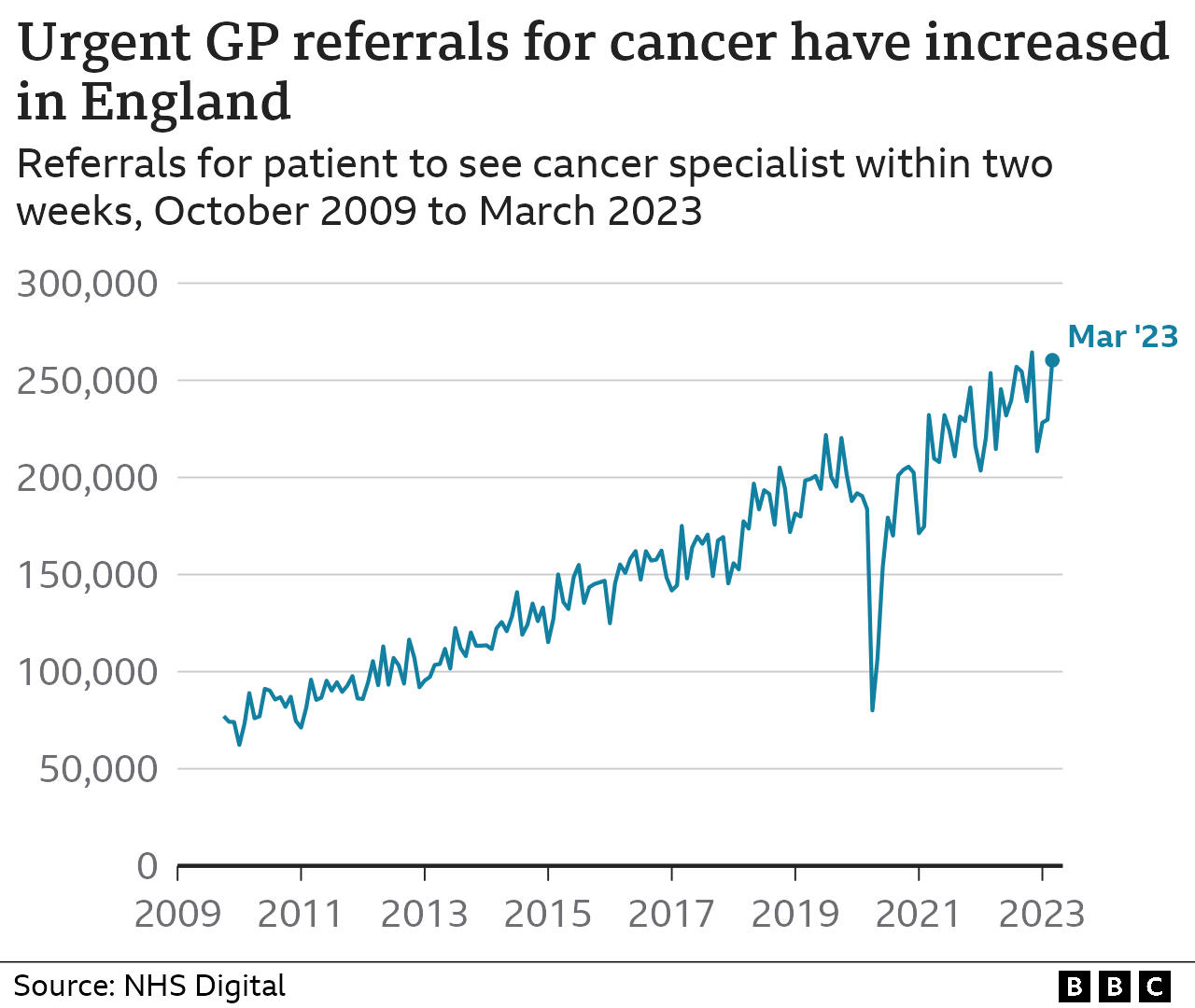
In the past ten years, there has been a marked increase in the number of people who seek medical attention after noticing a potential symptom like an odd lump, an odd mole, or unexplained weight loss.
The causes are numerous and include a rebound in demand following the implementation of Covid, stricter guidelines for GPs regarding the referral of patients to cancer specialists, significant NHS public relations initiatives, and the efforts of activists like "Bowelbabe" Deborah James.
Since more patients are now receiving earlier diagnoses when cancer is more treatable, oncologists see the increase in demand as a "very good thing.".
However, it also puts more strain on NHS services, with waiting times for diagnoses and other scans serving as a major system bottleneck.
Since Christmas, there have been some encouraging signs of improvement, with the English NHS cutting down on the backlog of patients who must wait an extended amount of time for treatment and finally meeting one of its other standards: quick diagnosis.
The RCR also notes a "chink of light" in the fact that oncologist hiring has increased over the past three years, particularly in regions of the nation with the worst staff shortages.
The report calls for more to be done to prevent experienced staff from reducing their hours or quitting their jobs early, as well as more medical school spots and training positions to be added in each UK nation.
According to the Department of Health, the total number of full-time employees working in the cancer field in England has increased by 51% to 33,093 since 2010.
A spokesperson continued, "We want to build on this progress and will soon publish a workforce plan to make sure we have the right number of employees with the right kind of skills. ".
The Scottish government is also anticipated to release its new 10-year cancer strategy in the coming weeks, which will outline strategies for hiring and retaining more personnel.
In a recently released cancer improvement plan, the Welsh government claims that it is currently investing heavily in staff training and the construction of additional diagnostic and treatment facilities. .
The health department in Northern Ireland described it as "extremely disappointing" that cancer prevention goals aren't being met. It recently started a "cancer strategy workforce review" and opened two new rapid diagnostic centers.
By Liana Bravo, data visualization.
Jim, please. via Twitter.







