A "historic" 15-year plan to address the NHS's staffing shortages will see a significant increase in the number of training spots for healthcare professionals in England.
Additionally, it places a greater emphasis on apprenticeships and adds more university spots for medical and nursing students, as well as the first-ever program for doctors.
There will also be a consultation on the possibility of one-year cuts to five-year medical degrees.
It took longer than anticipated to publish the plan—more than a year longer.
Since then, there have been numerous strikes affecting the NHS, and the conflict with the doctors is still raging.
The plan does not address pay; instead, it focuses on the need for more training spaces.
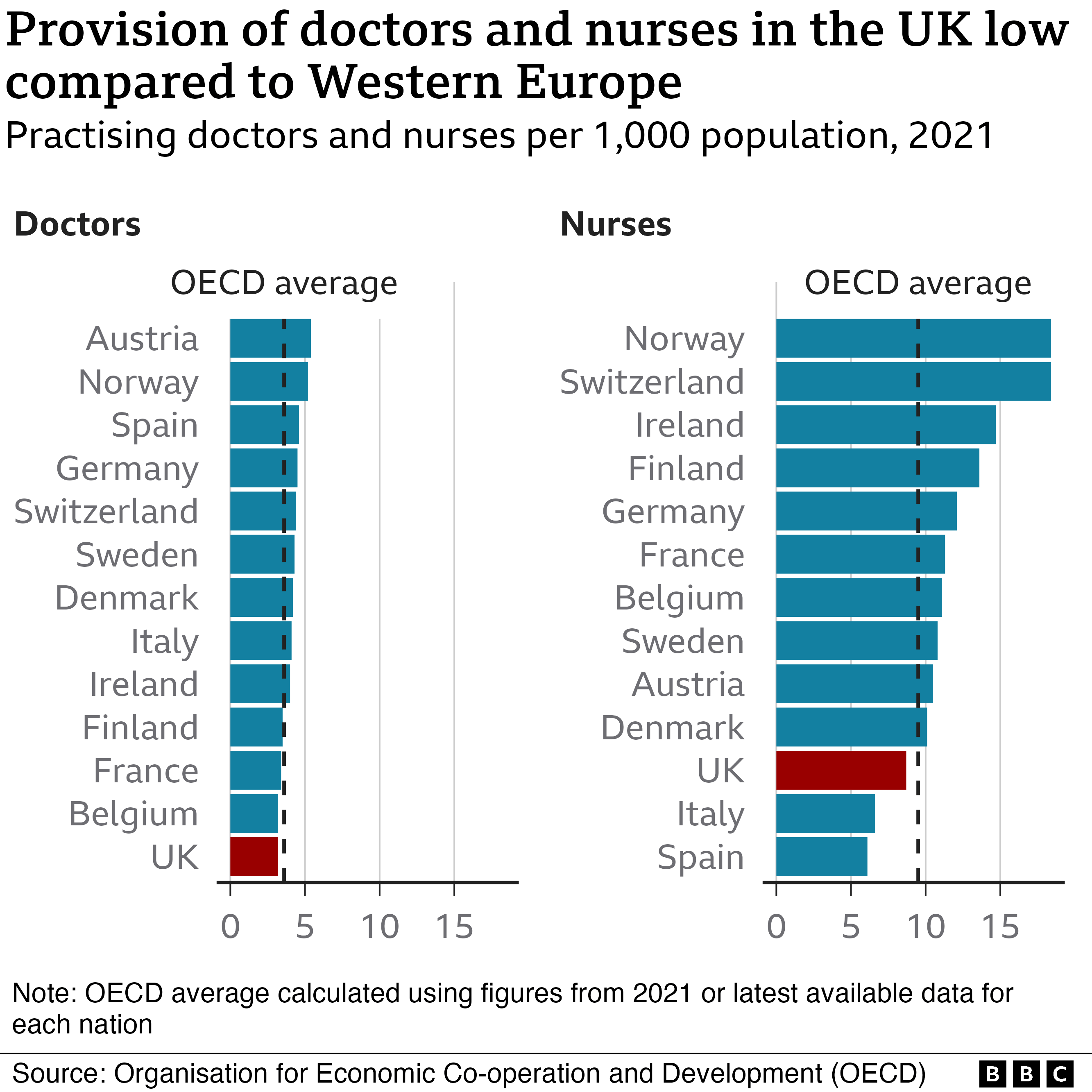
Due to the UK supply route's difficulty keeping up with demand, half of all new doctors and nurses must currently be recruited from abroad.
More than 110,000 open positions, or one out of every ten, remain unfilled.
And according to modeling for the plan, if nothing is done, this could increase to 360,000 by 2037.
The plan will be formally unveiled on Friday by the prime minister, Rishi Sunak, and the chief executive of NHS England, Amanda Pritchard.
The government has committed $21 billion over the following five years to aid in the goals' achievement.
It was a "historic" time, according to Ms. Pritchard, for the NHS.
We have a once-in-a-generation opportunity to put staffing on a solid foundation for the future because of it, she continued.
It was "one of the most important commitments," according to Mr. Sunak, that he would make as prime minister.
The objectives for 2031 are:.
- increasing the number of medical school spots available to 15,000 per year for future doctors.
- a 50% increase in the number of positions for junior doctors to train as GPs.
- Nearly twice as many nurse and midwifery student positions are added each year, at 24,000 more.
One out of every six NHS employees will have received their training through an apprenticeship in the next five years, including physiotherapists, podiatrists, and maternity staff. Apprenticeships combine paid work with academic study and do not require students to pay tuition.
A doctor apprenticeship program will begin the following year with a limited number of spots.

Thousands of people have already begun nursing apprenticeships, including Gemma Petters, who began hers at the Royal Derby Hospital in 2016 at the age of 30.
She claims, "I graduated from school not knowing what to do. "I worked at many different jobs. ".
As a nursing associate, a position that sits between a healthcare assistant and a nurse, Ms. Petters has now earned her certification.
The two years of nursing school will begin as her next step.
Ms. Petters claims that learning on the job has been extremely helpful.
We are becoming more familiar with the NHS's ethos and the needs of our patients, she says.
Additionally, it's crucial that she earn money as she studies.
Ms. Petters says, "I've got kids and a house to run.". "The security is really crucial and has given me the opportunity to pursue a career in the NHS. ".
There will also be a strong focus on employee retention, including more flexible work arrangements and career development to offer clear paths to senior positions. A record number of nurses left the NHS last year—more than 40,000.
Many people in the health service are supportive of the plan.
Health trust representative Matthew Taylor of the NHS Confederation referred to it as "bold and ambitious.".
The social care workforce now required the same level of dedication, he continued.
Others have noted that the effort to increase training spots may be hampered by the lack of front-line placements since a nurse student's degree involves working in the NHS for half of the time.
A medical degree takes five years to earn, while a nursing degree takes three. As a result, it will be years before this expansion begins to affect the current shortages.
Despite the plan's publication, Dr. Billy Palmer of the Nuffield Trust think tank said there had been "years of drift.".
He also cautioned that the current "dismal reality" of working in the NHS could jeopardize efforts to address shortages in the long run.
There is a chance that as more people are trained, they will become more and more exhausted, according to Dr. Palmer.
Wes Streeting, the shadow health secretary for Labour, stated that the government should have taken this action ten years ago if they had wanted the NHS to have enough staff members today.
. "







