A shortage of staff with the necessary skills was one of the big obstacles in resettling the patients of a hospital unit for vulnerable people, a psychiatrist has said.
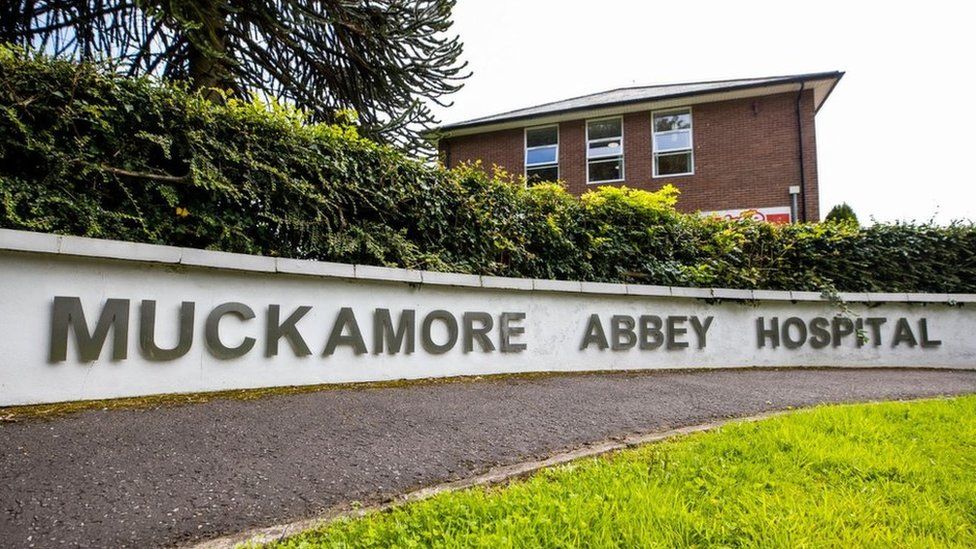
Muckamore Abbey Hospital in County Antrim is run by the Belfast Health Trust and provides facilities for adults with special needs.
It is at the centre of a public inquiry into alleged abuse of patients.
On Tuesday the inquiry heard that the unit had difficulty recruiting staff.
It was challenging to give patients the right care, according to Dr. Joanne Dougherty, who worked in training positions at Muckamore Abbey Hospital in 2007 and 2010.
"There's obviously a very specific, specialised skill mix required which often does need a lot of experience [of] actually working in this area and working with patients with these types of difficulties," said Dr Dougherty.
"So that's what I understand.
She told the inquiry that in meetings held between care managers from health trusts and the hospital's clinical team she often heard about the barriers for resettling patients who no longer needed inpatient care.
"I got the sense very much. the community services possibly were not developed sufficiently to meet the needs of highly-complex patients," she said.

Dr Dougherty said concerns were raised about securing appropriate physical space for patients and finding buildings in locations that offered reasonable access to other services.
In particular, the process of purchasing, hiring or leasing spaces for patients had been hampered, she said.
New-build schemes to meet the needs of patients had also been proposed.
Another issue was balancing the mix of patients who could live together comfortably, and what adaptations may be needed to allow for that to happen.
During questioning, Dr Dougherty was asked about the structures the other health trusts used to raise safeguarding issues in relation to their patients who were sent to Muckamore Abbey Hospital.
After 2019 inpatient teams at the hospital would meet staff from the patient's trust of origin on a daily basis to build an accurate and appropriate treatment plan.
Incidents in their care such as physical restraints, seclusion and interventions, would have been discussed in the hope of progressing a patient through hospital care to resettlement back into the community.
Dr Dougherty said prior to the change in 2019 those incidents may have been reported on a daily basis, depending on their nature.
However she said she was not sure if it was discussed during weekly meetings between clinical staff.
. that was proving quite difficult to achieve. "